A Detailed Guide from Good Care Home Health Services
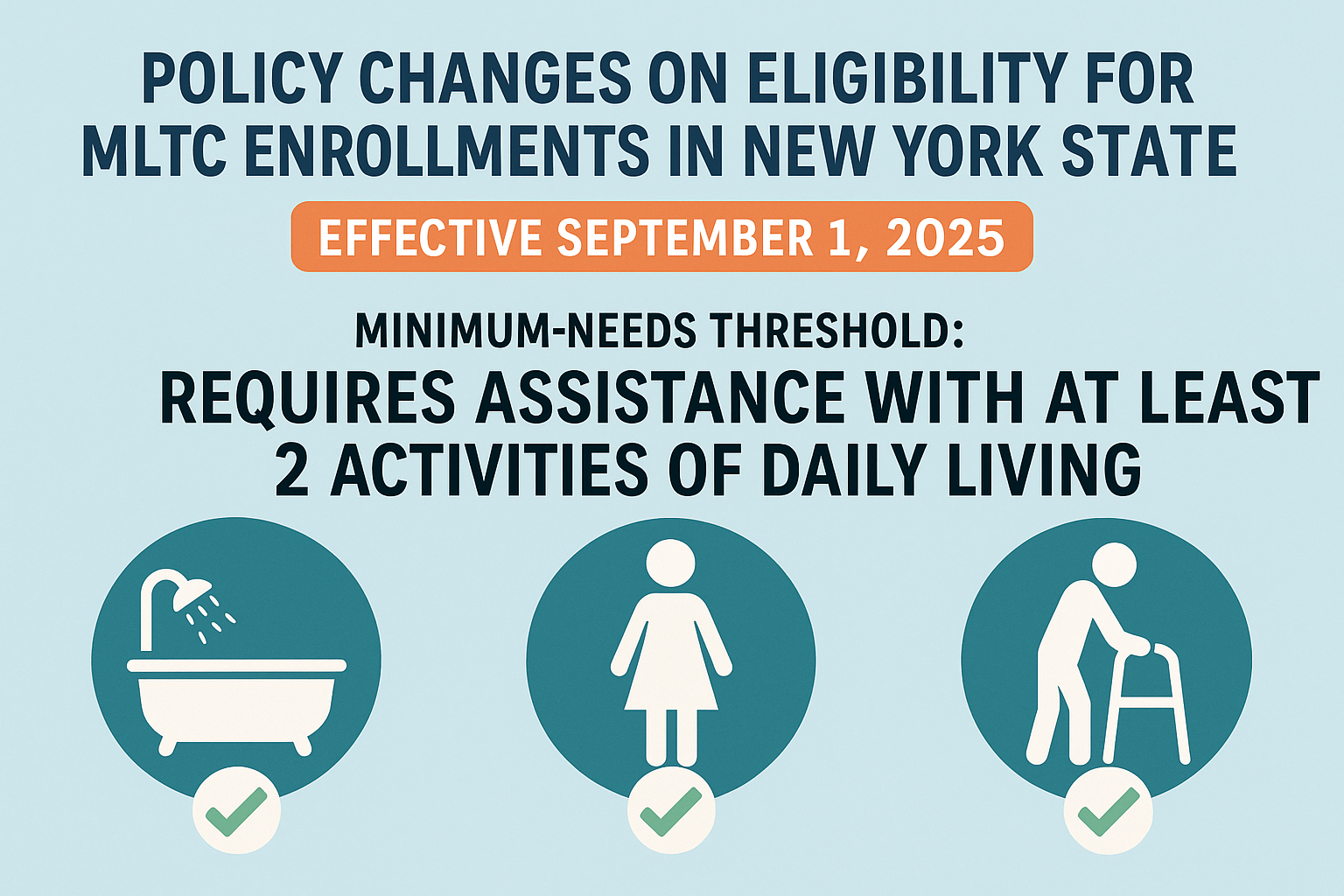
On September 1, 2025, a major policy change from the New York State Department of Health (DOH) will significantly tighten eligibility requirements for individuals applying to Managed Long Term Care (MLTC) and Medicaid Advantage Plus (MAP) plans. These changes are part of MLTC Policy 25.04, and they introduce a stricter standard known as the “Minimum Needs Requirement.”
This shift will impact:
Who qualifies for home care services through MLTC or MAP plans
What type of documentation is required
How assessments are conducted
How home care agencies manage intake, referrals, and ongoing client eligibility
At Good Care Home Health Services, we believe it's critical to educate our patients, families, referral partners, and care providers about these upcoming changes well in advance, so you can make informed decisions and avoid care disruptions.
🔍 What Is Changing?
Starting September 1, 2025, new applicants for MLTC and MAP will be required to meet stricter criteria than before. While the current rules only require an individual to need 120 days of community-based long-term care services (CBLTSS), the new rules add a second layer of clinical need.
Under the New Rule, You Must:
Be assessed as needing CBLTSS for more than 120 days, AND
Meet one of the following Minimum Needs Requirements:
Require at least limited physical assistance with more than two Activities of Daily Living (ADLs) OR
Have a documented diagnosis of Alzheimer’s or Dementia, and require at least supervision with more than one ADL
Common ADLs include:
Bathing
Dressing
Toileting
Transferring (e.g., from bed to chair)
Walking or mobility
Eating or feeding
This represents a significant change—especially for individuals who previously qualified based on supervision needs alone, such as cognitive or memory issues without a formal diagnosis.
🧠 Alzheimer’s and Dementia: New Documentation Requirements
Patients who are relying on a dementia-related diagnosis to qualify under the new rules must now submit specific documentation at every assessment.
To meet the dementia-based criteria:
The patient must use form DOH-5821 (Alzheimer’s or Dementia Documentation Form)
The diagnosis must include:
Patient’s full name and date of birth
Diagnosis and ICD-10 code
Name and license number of the diagnosing physician
The physician must be an M.D. or D.O.—but does not need to be Medicaid-enrolled
The form can be filled out by other licensed healthcare professionals (NP, PA, etc.) but the diagnosis itself must be made by a physician
📌 Without this documentation, individuals cannot qualify using the dementia pathway.
🕰️ Legacy Status: Why Enrolling Before September 1, 2025 Is So Important
One of the most significant features of the new policy is the introduction of “Legacy Status.” This provision allows individuals who enroll before the new rule takes effect to continue under the current (more flexible) eligibility rules, even after September 1, 2025.
You will be granted Legacy Status if:
You are enrolled in an MLTC or MAP plan before September 1, 2025
You were assessed between August 31, 2024 and August 31, 2025, and you enroll within one year of the assessment date
You had a scheduled assessment before September 1, 2025, which was rescheduled through no fault of your own and you enroll within one year
Once you are granted Legacy Status:
You will continue to be reassessed using pre-September 1, 2025 criteria
You are not required to meet the new Minimum Needs Requirements
No dementia documentation will be required if you qualified without it originally
⚠️ However, if you disenroll from your MLTC plan, you will lose Legacy Status, and any new application will be subject to the stricter new criteria
📋 What If You're Already Receiving Home Care?
If you are already receiving services through MLTC, MAP, CDPAS, or PCS before September 1, 2025:
You will be classified under Plan Legacy Status and/or Service Legacy Status
Your future reassessments will follow Legacy Criteria
You will not need to meet the new Minimum Needs Requirements
However, it’s critical that you do not allow your enrollment to lapse, as this will permanently remove your Legacy protections.
👥 Who Is Most At Risk of Losing Access?
The upcoming changes will especially impact:
Older adults with mild cognitive impairment or undiagnosed dementia
Individuals who only need supervision for safety, prompting, or memory support
Those without a formal diagnosis or physician documentation
Families who are delaying applying due to uncertainty or lack of awareness
We strongly advise all families who believe their loved one may need care in the next 6 to 12 months to begin the intake and assessment process now.
🏥 What Home Care Providers Must Do
As a licensed home care agency, Good Care Home Health Services is already preparing our team and partners for this transition. Here’s what providers must begin doing immediately:
✅ Train intake and assessment staff on the new eligibility rules
✅ Ensure they understand and can explain Minimum Needs Requirements
✅ Update internal workflows to track assessment and enrollment dates
✅ Begin pre-screening patients for legacy eligibility
✅ Educate referral partners (e.g., hospitals, social workers) on the September 1 deadline
✅ Guide families to gather necessary medical documentation, especially for dementia
Home care agencies will also need to work closely with the New York Independent Assessor Program (NYIAP) to schedule and validate assessments that may qualify for Legacy Status.
📅 Key Deadlines and Action Steps
Patients and Families:
✅ Apply now if you anticipate needing long-term care in the next year
✅ Request a NYIAP assessment before September 1, 2025
✅ Gather dementia/Alzheimer’s diagnosis documentation if applicable
✅ Enroll before the deadline to secure Legacy Status and avoid denial
Providers and Referral Sources:
📣 Communicate changes to all staff and patient families
🗂️ Track assessment dates to determine Legacy eligibility windows
🩺 Work with physicians to ensure proper completion of the DOH-5821 form
🔄 Monitor client reassessments and maintain Legacy Status in UAS-NY
🧭 Good Care Home Health Services Is Here to Help
We know these changes may seem overwhelming. That’s why Good Care is already:
Offering pre-enrollment consultations
Helping families gather medical documentation
Coordinating with MLTC plans and NYIAP
Monitoring all assessment timelines to preserve Legacy eligibility
Preparing our care coordinators to ensure no one is left behind
With over 25 years of experience in supporting patients throughout New York, we’re your trusted guide through this transition.
📞 Call Now – Don’t Wait Until It’s Too Late
If you or a loved one is considering home care services through Medicaid, act now to protect your eligibility.
🗓️ Deadline to enroll under current rules: August 31, 2025 After this date, many individuals will no longer qualify for MLTC or MAP services without more complex documentation and functional limitations.
📲 Contact Good Care Home Health Services today to begin the intake and eligibility process.